Introduction to Heart Valve Disease:
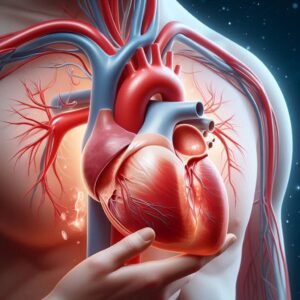
Heart valve disease is a significant and often debilitating condition that affects the proper functioning of the heart’s valves, which are crucial for directing blood flow through the heart and ensuring it moves efficiently to the rest of the body. The heart has four main valves: the aortic, mitral, tricuspid, and pulmonary valves.
Each valve plays a pivotal role in maintaining the unidirectional flow of blood. When any of these valves fail to operate correctly, it can lead to a range of health problems, from minor symptoms to life-threatening complications.
Heart valve disease can result from various factors, including congenital defects, age-related changes, infections, and other medical conditions such as high blood pressure and high cholesterol. Symptoms of heart valve disease can vary widely, from subtle signs like fatigue and shortness of breath to more severe manifestations such as chest pain and fainting spells.
Diagnosing this condition typically involves a combination of physical examinations and advanced imaging techniques like echocardiograms and MRIs. Treatment options range from lifestyle changes and medications to more invasive procedures like valve repair or replacement surgeries.
The impact of heart valve disease on a person’s quality of life and overall health underscores the importance of early detection and comprehensive management. Understanding the complexities of heart valve disease, recognizing its symptoms, and seeking timely medical intervention can significantly improve outcomes and help individuals lead healthier lives.

Heart valve disease is a medical condition that arises when one or more of the heart’s valves do not function properly. The heart contains four main valves—the aortic, mitral, tricuspid, and pulmonary valves—that play critical roles in regulating blood flow through the heart’s chambers and ensuring it is pumped efficiently to the rest of the body.
These valves open and close with each heartbeat, maintaining a one-way flow of blood and preventing backflow. When a valve becomes damaged or diseased, it can disrupt this flow, leading to two primary issues: stenosis and regurgitation. Stenosis occurs when a valve narrows, limiting the amount of blood that can pass through.
Regurgitation, on the other hand, happens when a valve does not close properly, allowing blood to leak backward. These malfunctions can strain the heart, reduce its efficiency, and cause a variety of symptoms, ranging from mild to severe.
The causes of heart valve disease are diverse and can include congenital defects present at birth, infections such as rheumatic fever and endocarditis, degenerative changes due to aging, and other medical conditions like hypertension and high cholesterol.
Diagnosing heart valve disease involves thorough medical evaluations, including listening for heart murmurs, which can indicate abnormal blood flow, and using imaging tests like echocardiograms, ECGs, and MRIs to visualize the heart’s structure and function.
Treatment depends on the severity of the condition and may involve medications to manage symptoms, lifestyle changes to improve heart health, or surgical interventions to repair or replace the affected valve. Understanding heart valve disease is crucial for managing its symptoms and preventing complications, highlighting the importance of early detection and appropriate medical care.
Types of Heart Valve Disease:
Heart valve disease encompasses several distinct conditions, each affecting one of the heart’s four valves: the aortic, mitral, tricuspid, and pulmonary valves. Each type of valve disease presents unique challenges and symptoms, depending on which valve is affected and how it is malfunctioning.
Aortic valve disease, one of the most common forms, includes aortic stenosis, where the valve narrows, obstructing blood flow from the heart to the aorta, and aortic regurgitation, where the valve fails to close properly, causing blood to leak back into the heart.
Mitral valve disease involves issues with the mitral valve, such as mitral stenosis, a narrowing that impedes blood flow from the left atrium to the left ventricle, and mitral regurgitation, where the valve allows blood to flow backward into the left atrium.
Mitral valve prolapse, another common condition, occurs when the valve’s flaps bulge into the atrium during contraction, potentially leading to regurgitation. Tricuspid valve disease affects the tricuspid valve, including tricuspid stenosis, a rare condition that restricts blood flow from the right atrium to the right ventricle, and tricuspid regurgitation, where blood leaks back into the right atrium.
Pulmonary valve disease involves the pulmonary valve and includes pulmonary stenosis, a narrowing that hampers blood flow from the right ventricle to the pulmonary artery, and pulmonary regurgitation, where the valve allows blood to flow back into the right ventricle.
These conditions can be congenital, present from birth, or acquired due to factors such as infections, age-related changes, or other health issues. Each type of valve disease requires careful diagnosis and management to prevent complications and maintain heart health, emphasizing the importance of understanding the specific characteristics and treatment needs of the different forms of heart valve disease.
Aortic Valve Disease:
Aortic valve disease is a significant condition that primarily affects the aortic valve, one of the heart’s crucial components responsible for regulating blood flow from the left ventricle into the aorta, the largest artery in the body. This disease manifests in two main forms: aortic stenosis and aortic regurgitation.
Aortic stenosis occurs when the aortic valve narrows, often due to calcification and thickening of the valve tissue, which restricts blood flow and forces the heart to work harder to pump blood through the narrowed opening. This increased workload can lead to symptoms such as chest pain, fainting, shortness of breath, and heart failure if left untreated.
Aortic regurgitation, on the other hand, happens when the aortic valve does not close properly, allowing blood to leak back into the left ventricle after it has been pumped out, which can cause the heart to enlarge and weaken over time.
Causes of aortic valve disease can include congenital defects like bicuspid aortic valve, rheumatic fever, endocarditis, and degenerative changes related to aging. Diagnosis often involves a combination of physical examinations, where doctors listen for heart murmurs, and advanced imaging techniques such as echocardiograms, which provide detailed images of the valve’s structure and function.
Treatment options vary depending on the severity of the disease and can range from medications to manage symptoms and slow progression to surgical interventions like aortic valve repair or replacement. Valve replacement can be done using either mechanical valves, which are durable but require lifelong blood thinners, or biological valves, which have a more natural function but may need to be replaced after a certain period.
With advances in medical technology, minimally invasive procedures such as transcatheter aortic valve replacement (TAVR) have become more common, offering a less invasive alternative to open-heart surgery. Understanding aortic valve disease is crucial for timely intervention and management, helping patients maintain a better quality of life and preventing severe complications.
Mitral Valve Disease:
Aortic valve disease is a significant condition that primarily affects the aortic valve, one of the heart’s crucial components responsible for regulating blood flow from the left ventricle into the aorta, the largest artery in the body. This disease manifests in two main forms: aortic stenosis and aortic regurgitation.
Aortic stenosis occurs when the aortic valve narrows, often due to calcification and thickening of the valve tissue, which restricts blood flow and forces the heart to work harder to pump blood through the narrowed opening.
This increased workload can lead to symptoms such as chest pain, fainting, shortness of breath, and heart failure if left untreated. Aortic regurgitation, on the other hand, happens when the aortic valve does not close properly, allowing blood to leak back into the left ventricle after it has been pumped out, which can cause the heart to enlarge and weaken over time.
Causes of aortic valve disease can include congenital defects like bicuspid aortic valve, rheumatic fever, endocarditis, and degenerative changes related to aging. Diagnosis often involves a combination of physical examinations, where doctors listen for heart murmurs, and advanced imaging techniques such as echocardiograms, which provide detailed images of the valve’s structure and function.
Treatment options vary depending on the severity of the disease and can range from medications to manage symptoms and slow progression to surgical interventions like aortic valve repair or replacement. Valve replacement can be done using either mechanical valves, which are durable but require lifelong blood thinners, or biological valves, which have a more natural function but may need to be replaced after a certain period.
With advances in medical technology, minimally invasive procedures such as transcatheter aortic valve replacement (TAVR) have become more common, offering a less invasive alternative to open-heart surgery. Understanding aortic valve disease is crucial for timely intervention and management, helping patients maintain a better quality of life and preventing severe complications.
Tricuspid Valve Disease:
Tricuspid valve disease is a condition that affects the tricuspid valve, which is located between the right atrium and the right ventricle of the heart. This valve is crucial for controlling blood flow from the right atrium to the right ventricle and preventing backflow when the ventricle contracts.
Tricuspid valve disease can present in two primary forms: tricuspid stenosis and tricuspid regurgitation. Tricuspid stenosis is characterized by a narrowing of the tricuspid valve, which restricts blood flow from the right atrium to the right ventricle.
This condition can lead to increased pressure in the atrium and veins, resulting in symptoms such as fatigue, swelling in the legs and abdomen, and liver enlargement. Tricuspid regurgitation, the more common form of the disease, occurs when the tricuspid valve does not close properly, allowing blood to flow backward into the right atrium each time the right ventricle contracts.
This can cause the right atrium to enlarge and the right ventricle to become overworked, leading to symptoms like fatigue, irregular heart rhythms, and fluid retention in the lower extremities and abdomen.
Tricuspid valve disease can arise from various causes, including congenital defects, rheumatic fever, endocarditis, and damage from previous heart surgery or radiation therapy. It is often associated with other heart conditions, such as left-sided heart valve diseases or pulmonary hypertension, which increase the pressure the right side of the heart must manage.
Diagnosing tricuspid valve disease typically involves a combination of physical examinations, where physicians listen for abnormal heart sounds, and imaging tests like echocardiograms, which provide detailed visuals of the valve’s function and structure. Treatment depends on the severity of the condition and the underlying cause.
Mild cases may be managed with medications to reduce symptoms and prevent further complications, while more severe cases might require surgical intervention. Surgical options include valve repair, where the existing valve is modified to function more effectively, or valve replacement, where the damaged valve is replaced with a mechanical or biological substitute.
Advances in medical technology have also introduced less invasive procedures, such as transcatheter tricuspid valve repair (TTVR), offering alternatives to traditional open-heart surgery. Proper management of tricuspid valve disease is essential to prevent serious complications like heart failure and to improve the quality of life for those affected.
Pulmonary Valve Disease:
Pulmonary valve disease is a condition that affects the pulmonary valve, which is responsible for regulating blood flow from the right ventricle to the pulmonary artery, leading to the lungs for oxygenation. This disease can manifest in two primary forms: pulmonary stenosis and pulmonary regurgitation.
Pulmonary stenosis occurs when the pulmonary valve is narrowed, obstructing blood flow from the right ventricle to the pulmonary artery. This obstruction forces the right ventricle to work harder to pump blood, potentially leading to right ventricular hypertrophy (thickening of the heart muscle) and symptoms such as shortness of breath, chest pain, and fatigue.
Pulmonary regurgitation, on the other hand, happens when the pulmonary valve does not close properly, allowing blood to flow back into the right ventricle after it has been pumped out. This backflow can cause the right ventricle to dilate and weaken over time, resulting in symptoms like fatigue, swelling in the legs and abdomen, and heart palpitations.
Pulmonary valve disease can be congenital, meaning it is present at birth, often due to malformations during fetal development, or it can be acquired due to conditions such as carcinoid syndrome, rheumatic fever, or previous heart surgery.
Diagnosis typically involves physical examinations and imaging tests like echocardiograms, which provide detailed images of the valve’s structure and function. Treatment options depend on the severity of the disease and can range from regular monitoring and medications to manage symptoms to surgical interventions.
Surgical procedures may include balloon valvuloplasty, where a balloon is used to open a narrowed valve, or valve replacement, where the damaged valve is replaced with a biological or mechanical one.
Advances in minimally invasive techniques, such as transcatheter pulmonary valve replacement (TPVR), offer less invasive alternatives to traditional surgery. Managing pulmonary valve disease effectively is crucial for maintaining heart function and preventing complications, allowing individuals to lead healthier, more active lives.
Causes of Heart Valve Disease:
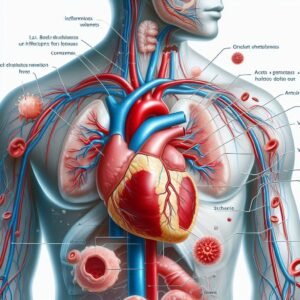
Heart valve disease can arise from a variety of causes, ranging from congenital defects to acquired conditions. Congenital heart defects, present at birth, are a common cause and often involve malformations of one or more heart valves that impede their normal function.
These defects can lead to issues such as valve stenosis or regurgitation. Age-related changes are another significant cause, as the wear and tear on the heart valves over time can lead to conditions like calcification, where the valve tissues thicken and stiffen, restricting proper blood flow.
Infections, particularly rheumatic fever and infective endocarditis, can damage the heart valves, leading to scarring and functional impairments. Rheumatic fever, a complication of untreated strep throat, can cause long-term damage to the heart valves, while infective endocarditis involves bacterial infection of the valve tissues, resulting in inflammation and destruction.
Other medical conditions, such as high blood pressure, high cholesterol, and atherosclerosis, can also contribute to heart valve disease by increasing the strain on the heart and promoting changes in the valve structures.
Additionally, certain autoimmune diseases like lupus can lead to valve inflammation and dysfunction. Lifestyle factors, including poor diet, lack of exercise, and smoking, can exacerbate these conditions and increase the risk of developing heart valve disease. Understanding these various causes is essential for prevention, early detection, and effective management of heart valve disease.
Congenital Heart Defects:
Congenital heart defects are structural abnormalities present in the heart at birth, affecting its chambers, valves, or blood vessels. These defects develop during fetal growth and can vary widely in severity, from minor issues that may not require treatment to complex conditions that can be life-threatening without intervention.
Some common congenital heart defects include atrial septal defects, where there is a hole between the heart’s upper chambers (atria), ventricular septal defects, where there is a hole between the heart’s lower chambers (ventricles), and tetralogy of Fallot, a combination of defects that affect the heart’s structure and blood flow.
The exact cause of congenital heart defects is often unknown, although genetic factors, maternal infections during pregnancy, and exposure to certain substances or medications may play a role. Diagnosis typically occurs during prenatal ultrasounds or shortly after birth, through physical examinations and imaging tests.
Treatment options depend on the type and severity of the defect but may include medications, catheter-based interventions, or surgery to repair or correct the abnormality. With advances in medical technology and improved surgical techniques, many individuals with congenital heart defects can lead full and active lives with appropriate management and care.
Age-Related Changes:
As individuals age, their heart valves undergo natural changes that can increase the risk of developing heart valve disease. One of the most common age-related changes is the thickening and stiffening of the valve tissues, a condition known as calcification.
This calcification makes the valves less flexible and can impair their ability to open and close properly, leading to conditions like valve stenosis or regurgitation. Additionally, wear and tear on the heart valves over time can cause degenerative changes, such as the formation of nodules or lesions on the valve surfaces, which can further compromise their function.
Age-related changes can also affect the connective tissues that support the heart valves, leading to alterations in their structure and integrity. While these changes are a natural part of the aging process, they can increase the risk of developing heart valve disease, particularly in older adults.
Regular medical checkups and monitoring are essential for detecting age-related changes in the heart valves early and implementing appropriate interventions to prevent or manage heart valve disease effectively.
Infections:
Infections like endocarditis pose a significant risk to heart valve health, as they can lead to damage and dysfunction of the heart valves. Endocarditis is an infection of the inner lining of the heart chambers and valves, often caused by bacteria entering the bloodstream and attaching to the heart’s surfaces.
When bacteria settle on heart valves, they can cause inflammation, scarring, and even destruction of the valve tissue, compromising its ability to function properly. As a result, affected valves may develop leaks (regurgitation) or become narrowed (stenosis), impairing blood flow and potentially leading to serious complications such as heart failure or stroke.
Prompt diagnosis and treatment of endocarditis are crucial to prevent irreversible damage to the heart valves and preserve overall heart function.
Symptoms of Heart Valve Disease:
Symptoms of heart valve disease can vary depending on the type and severity of the condition. In the early stages, individuals may experience subtle signs such as fatigue, shortness of breath during physical activity, or a general feeling of weakness.
As the disease progresses, more pronounced symptoms may develop, including chest pain or discomfort, particularly during exertion or when lying flat, palpitations or irregular heartbeats, fainting or lightheadedness, and swelling in the ankles, feet, or abdomen due to fluid retention.
Additionally, some individuals may experience a persistent cough, especially at night or when lying down, or notice a fluttering sensation in the chest.
Advanced symptoms can significantly impact daily life and may indicate a more severe form of heart valve disease that requires prompt medical attention. Recognizing these symptoms and seeking timely evaluation by a healthcare professional is crucial for proper diagnosis and management of heart valve disease.
Early Symptoms:
Early symptoms of heart valve disease can be subtle and easily overlooked, but they often serve as important warning signs of underlying issues with the heart valves.
These symptoms may include mild fatigue, especially during physical activity, shortness of breath or difficulty breathing, particularly when exerting oneself or lying flat, and a general feeling of weakness or lethargy.
Some individuals may also experience palpitations or irregular heartbeats, chest discomfort, or mild swelling in the ankles or feet. While these early symptoms may not be severe, they should not be ignored, as they could indicate the presence of heart valve disease or other cardiovascular conditions.
Seeking medical evaluation and timely intervention can help identify the underlying cause of these symptoms and prevent the progression of heart valve disease to more advanced stages.
Advanced Symptoms:
Advanced symptoms of heart valve disease often manifest as more pronounced and debilitating signs of cardiovascular dysfunction. Individuals with advanced heart valve disease may experience severe fatigue and weakness, even with minimal physical exertion. Shortness of breath can become more persistent and occur even at rest or with minimal activity.
Chest pain or discomfort may worsen and become more frequent, sometimes radiating to the neck, arms, or back. Palpitations or irregular heartbeats may become more pronounced and disruptive to daily life.
Additionally, individuals may experience episodes of fainting or lightheadedness, indicating inadequate blood flow to the brain. Swelling in the ankles, feet, or abdomen may become more severe as fluid retention increases due to heart failure. These advanced symptoms significantly impact quality of life and require immediate medical attention to prevent further complications and improve outcomes.
Diagnosis of Heart Valve Disease:
Diagnosis of heart valve disease involves a comprehensive assessment by healthcare professionals to accurately identify the condition and determine its severity. Physical examinations are often the first step, during which doctors listen for abnormal heart sounds, known as murmurs, using a stethoscope.
Additionally, healthcare providers may inquire about symptoms and medical history to better understand the patient’s overall health and potential risk factors for heart valve disease.
Following the initial assessment, imaging tests such as echocardiograms, electrocardiograms (ECGs), chest X-rays, and cardiac magnetic resonance imaging (MRI) may be performed to visualize the heart’s structure and function.
Echocardiograms, in particular, provide detailed images of the heart valves and chambers, allowing healthcare providers to assess valve movement, thickness, and any abnormalities. ECGs measure the heart’s electrical activity and can detect irregular rhythms associated with valve disease.
Chest X-rays and cardiac MRI provide additional information about the heart’s size, shape, and overall condition. Based on the findings from these tests, healthcare providers can make an accurate diagnosis of heart valve disease and develop an appropriate treatment plan tailored to the patient’s needs.
Physical Examination:
During a physical examination for heart valve disease, healthcare providers assess various aspects of cardiovascular health to identify any abnormalities or signs of valve dysfunction. Using a stethoscope, they listen for specific heart sounds, known as murmurs, which can indicate turbulent blood flow through the heart valves.
The presence, intensity, and location of murmurs provide valuable information about the type and severity of valve disease. Additionally, healthcare providers may evaluate other vital signs, such as blood pressure and pulse rate, to assess overall cardiac function.
They may also look for physical signs of heart valve disease, such as swelling in the legs or abdomen, which can indicate fluid retention due to heart failure. Through thorough examination and attention to detail, healthcare providers can gather essential clues about the patient’s cardiovascular health and determine the need for further diagnostic testing or intervention.
Diagnostic Tests:
Diagnostic tests play a crucial role in confirming the presence and severity of heart valve disease, providing valuable insights into the structure and function of the heart valves. These tests encompass a range of imaging techniques and cardiac evaluations designed to assess cardiac anatomy, blood flow, and valve function.
Echocardiography, including transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE), is a primary diagnostic tool used to visualize the heart valves and chambers in real-time, allowing healthcare providers to assess valve morphology, movement, and any abnormalities.
Electrocardiography (ECG) records the heart’s electrical activity, detecting irregular rhythms associated with valve disease. Other imaging modalities, such as cardiac MRI and CT scans, provide detailed images of the heart’s structure and function, aiding in diagnosis and treatment planning.
Additionally, cardiac catheterization and angiography may be used to assess blood flow through the heart and measure pressure within the chambers. By utilizing a combination of diagnostic tests, healthcare providers can accurately diagnose heart valve disease and develop personalized treatment strategies to optimize patient outcomes.
Echocardiogram:
An echocardiogram is a non-invasive diagnostic test that uses sound waves to create detailed images of the heart’s structure and function. During an echocardiogram, a small handheld device called a transducer is placed on the chest, emitting sound waves that bounce off the heart and are converted into moving images displayed on a monitor.
This imaging technique allows healthcare providers to visualize the heart valves, chambers, and blood flow patterns in real-time. Echocardiograms provide valuable information about the size, shape, and movement of the heart, as well as any abnormalities or defects in the heart valves or walls.
There are different types of echocardiograms, including transthoracic echocardiography (TTE), which is performed by placing the transducer on the chest, and transesophageal echocardiography (TEE), where the transducer is inserted into the esophagus for a closer view of the heart.
Echocardiograms are commonly used to diagnose and monitor heart valve disease, as well as other cardiac conditions, helping healthcare providers make informed decisions about treatment and management.
Electrocardiogram (ECG):
An electrocardiogram (ECG or EKG) is a common diagnostic test used to measure and record the electrical activity of the heart. During an ECG, electrodes are placed on the skin of the chest, arms, and legs, which detect and transmit the electrical signals produced by the heart as it beats.
These signals are then displayed as waves on a graph, providing valuable information about the heart’s rhythm, rate, and overall electrical conduction. An ECG can detect various abnormalities in the heart’s electrical activity, such as arrhythmias (irregular heartbeats), conduction disorders, and signs of myocardial ischemia or infarction (heart attack).
It is a quick and painless procedure that is often performed as part of routine cardiac assessments or in response to symptoms such as chest pain, palpitations, or dizziness. ECGs are valuable tools for diagnosing heart valve disease and other cardiac conditions, guiding treatment decisions, and monitoring the effectiveness of interventions over time.
Chest X-ray:

A chest X-ray is a common diagnostic imaging test used to evaluate the structures within the chest, including the heart and lungs. During a chest X-ray, a small dose of radiation is directed through the chest area, and the resulting images are captured on a specialized film or digital sensor.
These images provide detailed information about the size, shape, and position of the heart, as well as any abnormalities or conditions affecting the lungs, ribs, and surrounding structures.
In the context of heart valve disease, a chest X-ray may be performed to assess the overall size and shape of the heart, identify signs of heart enlargement or fluid accumulation in the lungs (pulmonary congestion), and detect any calcifications or abnormalities in the heart valves or surrounding tissues.
While a chest X-ray alone may not provide a definitive diagnosis of heart valve disease, it is a valuable tool for assessing cardiac and pulmonary health, guiding further diagnostic evaluations, and monitoring changes over time.
Cardiac MRI:
Cardiac MRI, or magnetic resonance imaging, is a sophisticated imaging technique used to create detailed images of the heart and its surrounding structures. Unlike other imaging modalities, such as X-rays or CT scans, cardiac MRI does not use ionizing radiation.
Instead, it relies on powerful magnets and radio waves to generate high-resolution images of the heart in multiple planes. Cardiac MRI provides comprehensive information about the heart’s size, shape, function, and blood flow patterns, making it a valuable tool for diagnosing and evaluating various cardiac conditions, including heart valve disease.
With cardiac MRI, healthcare providers can assess the morphology and function of the heart valves, detect any abnormalities or defects, and evaluate the impact of valve disease on overall cardiac function.
Additionally, cardiac MRI can help guide treatment decisions and monitor the effectiveness of interventions, such as valve repair or replacement surgery. Overall, cardiac MRI offers a non-invasive and highly accurate method for assessing heart valve disease and optimizing patient care.
Treatment Options for Heart Valve Disease:
Treatment options for heart valve disease depend on several factors, including the type and severity of the condition, as well as the individual’s overall health and preferences. In mild cases of heart valve disease, where symptoms are minimal and the risk of complications is low, conservative management strategies may be sufficient.
This approach may involve regular monitoring of the condition, lifestyle modifications such as dietary changes and exercise, and medications to alleviate symptoms and prevent complications. However, in more severe cases or when symptoms become debilitating, more aggressive treatment options may be necessary.
These options may include medications to manage symptoms, such as diuretics to reduce fluid buildup or beta-blockers to control heart rate and blood pressure. In some cases, minimally invasive procedures such as balloon valvuloplasty or transcatheter valve repair may be performed to improve valve function without the need for open-heart surgery.
However, for advanced cases of heart valve disease or when conservative treatments are ineffective, surgical interventions such as valve repair or replacement may be required.
During valve repair surgery, the damaged valve is repaired to improve its function, while in valve replacement surgery, the diseased valve is replaced with a mechanical or biological prosthetic valve.
The choice of treatment depends on various factors, including the patient’s age, overall health, and preference, as well as the type and severity of the valve disease. By working closely with a multidisciplinary healthcare team, individuals with heart valve disease can explore the various treatment options available and make informed decisions about their care to optimize outcomes and improve quality of life.
Medications:
Medications are an essential component of treatment for heart valve disease, often used to manage symptoms, improve heart function, and prevent complications. Several classes of medications may be prescribed depending on the specific needs of the individual and the type of valve disease they have.
Diuretics, such as furosemide or spironolactone, are commonly used to reduce fluid buildup in the body, alleviating symptoms like shortness of breath and swelling in the legs and abdomen.
Beta-blockers, such as metoprolol or carvedilol, may be prescribed to control heart rate and blood pressure, reducing the workload on the heart and improving symptoms like palpitations and chest pain.
Additionally, medications like ACE inhibitors or angiotensin receptor blockers (ARBs) may be used to lower blood pressure and improve heart function in individuals with heart valve disease and associated conditions such as hypertension.
Anticoagulants, such as warfarin or direct oral anticoagulants (DOACs), are often prescribed to reduce the risk of blood clots forming on damaged heart valves, particularly in individuals with mechanical valve replacements or atrial fibrillation.
Other medications, such as antiarrhythmics or antibiotics, may be used in specific cases to manage irregular heart rhythms or prevent infections of the heart valves, respectively. It is essential for individuals with heart valve disease to take their medications as prescribed by their healthcare provider and to attend regular follow-up appointments to monitor their condition and adjust treatment as needed.
Surgical Procedures:
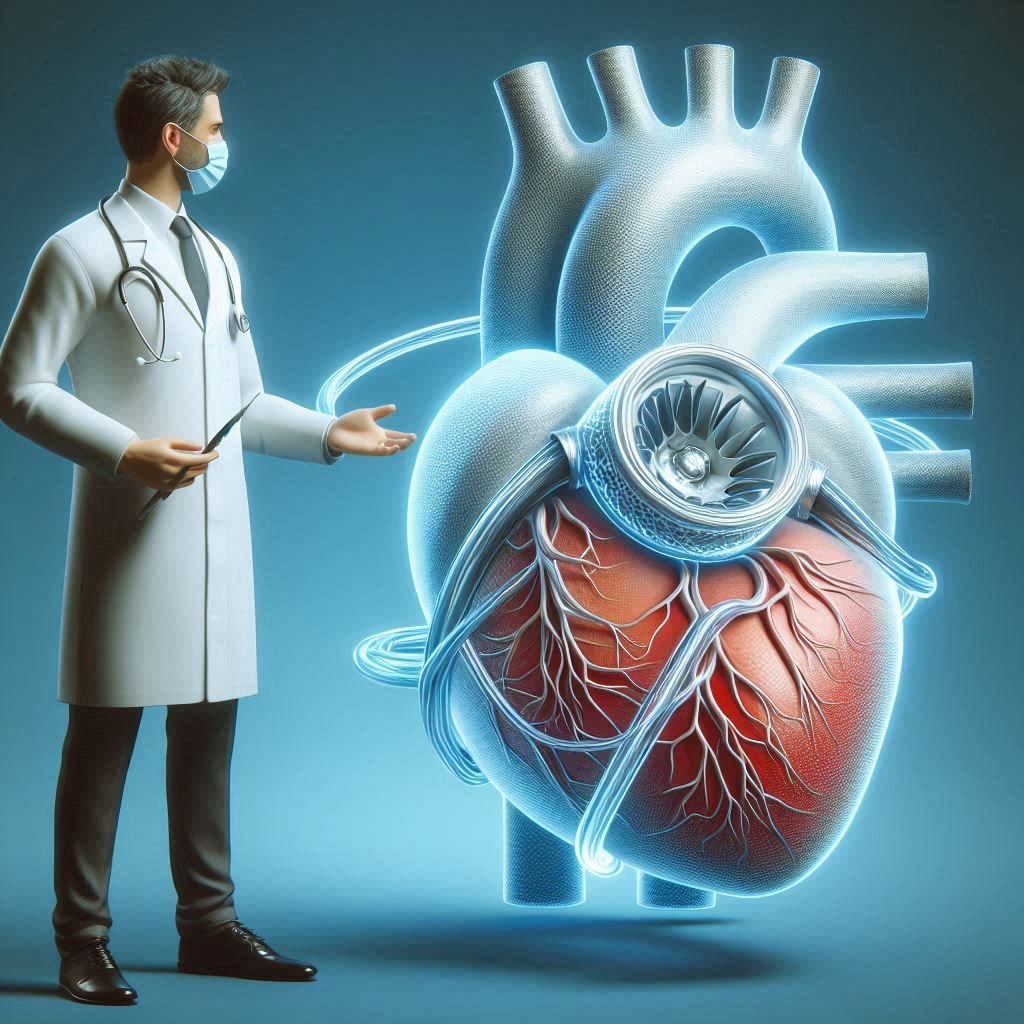
Surgical procedures play a crucial role in the treatment of heart valve disease, particularly in cases where conservative measures or minimally invasive interventions are insufficient to address the severity of the condition.
There are several types of surgical procedures commonly used to repair or replace damaged heart valves, depending on the specific valve involved, the extent of the damage, and the individual’s overall health status.
Valve repair surgery involves repairing the existing valve to restore its function and integrity. This may involve techniques such as valve reconstruction, patching, or resizing to correct structural abnormalities and improve valve function.
Valve replacement surgery, on the other hand, involves removing the diseased valve and replacing it with a prosthetic valve. There are two main types of prosthetic valves: mechanical valves, made of durable materials such as metal or carbon, and biological valves, made from animal tissue or human tissue obtained from organ donors.
Each type of valve has its advantages and disadvantages, and the choice of valve depends on various factors, including the individual’s age, lifestyle, and preference. Surgical procedures for heart valve disease may be performed using traditional open-heart surgery techniques or minimally invasive approaches, such as robotic-assisted surgery or transcatheter procedures.
Minimally invasive techniques offer the advantage of smaller incisions, reduced risk of complications, and quicker recovery times compared to traditional open-heart surgery. However, the suitability of these techniques depends on the specific characteristics of the valve disease and the expertise of the surgical team.
Overall, surgical procedures for heart valve disease are highly effective in improving symptoms, restoring cardiac function, and enhancing quality of life for individuals with this condition.
Valve Repair:
Valve repair is a surgical procedure aimed at restoring the function and integrity of a damaged heart valve without replacing it entirely. This procedure is often preferred when the valve damage is localized and repairable, preserving the native tissue and avoiding the need for prosthetic valve replacement.
Valve repair techniques vary depending on the specific valve involved and the nature of the damage. For example, in cases of mitral valve prolapse, where the valve’s flaps bulge into the atrium during contraction, repair may involve tightening or reshaping the valve tissue to improve its closure.
Similarly, in cases of tricuspid valve regurgitation, where the valve does not close properly, repair may involve techniques such as ring annuloplasty, where a ring-like device is placed around the valve to support and reinforce its structure.
Valve repair surgery offers several advantages over valve replacement, including preservation of the patient’s own tissue, reduced risk of complications such as infection or thrombosis, and avoidance of long-term anticoagulation therapy in some cases.
However, not all valve damage is amenable to repair, and the decision to repair or replace a valve depends on various factors, including the severity of the damage, the patient’s overall health status, and the expertise of the surgical team. Overall, valve repair is a valuable option for selected patients with heart valve disease, offering the potential for improved outcomes and long-term durability.
Valve Replacement:
Valve replacement is a surgical procedure performed to replace a damaged or diseased heart valve with a prosthetic valve. This procedure is typically recommended when the valve damage is severe and irreversible, making repair unfeasible or ineffective.
There are two main types of prosthetic valves used in valve replacement surgery: mechanical valves and biological valves. Mechanical valves are made of durable materials such as metal or carbon and are designed to last a lifetime.
However, individuals with mechanical valves require lifelong anticoagulation therapy to prevent blood clots from forming on the valve surface. Biological valves, on the other hand, are made from animal tissue or human tissue obtained from organ donors.
While biological valves do not require long-term anticoagulation therapy, they may wear out over time and need to be replaced. Valve replacement surgery can be performed using traditional open-heart surgery techniques or minimally invasive approaches, depending on the specific characteristics of the valve disease and the patient’s overall health status.
During the procedure, the damaged valve is removed, and the prosthetic valve is sewn into place. Valve replacement surgery offers several benefits, including improved symptoms, restored cardiac function, and enhanced quality of life for individuals with severe heart valve disease.
However, like all surgical procedures, valve replacement carries some risks, including bleeding, infection, and complications related to anesthesia. The choice of valve type and surgical approach depends on various factors, including the patient’s age, lifestyle, and preference, as well as the expertise of the surgical team.
Overall, valve replacement is a highly effective treatment option for individuals with advanced heart valve disease, offering the potential for long-term durability and improved outcomes.
Non-Surgical Procedures:
Non-surgical procedures offer less invasive alternatives to traditional open-heart surgery for the treatment of heart valve disease. These procedures are often performed using catheter-based techniques, which involve threading a thin, flexible tube (catheter) through blood vessels to access the heart and perform interventions.
One common non-surgical procedure for heart valve disease is balloon valvuloplasty, which is used to treat valve stenosis by widening a narrowed valve opening. During the procedure, a balloon-tipped catheter is inserted into the narrowed valve and inflated, stretching the valve tissue and improving blood flow.
Another minimally invasive technique is transcatheter valve repair or replacement, which involves implanting a prosthetic valve using a catheter-based approach. This procedure is particularly beneficial for individuals who are at high risk for complications from traditional surgery or who are not suitable candidates for open-heart surgery due to underlying health conditions.
Transcatheter procedures are typically performed in a specialized cardiac catheterization laboratory (cath lab) under imaging guidance, such as fluoroscopy or echocardiography. While non-surgical procedures offer several advantages, including shorter recovery times, reduced risk of complications, and avoidance of sternotomy (chest incision), they may not be suitable for all patients or all types of valve disease.
The choice of procedure depends on various factors, including the specific characteristics of the valve disease, the patient’s overall health status, and the expertise of the medical team. Overall, non-surgical procedures provide valuable treatment options for individuals with heart valve disease, offering the potential for improved symptoms and quality of life with minimal invasiveness.
Preventing Heart Valve Disease:
Preventing heart valve disease involves adopting healthy lifestyle habits and managing underlying risk factors to maintain optimal heart health. One key aspect of prevention is controlling conditions that can contribute to valve damage, such as high blood pressure, high cholesterol, and diabetes.
This can be achieved through regular exercise, a balanced diet rich in fruits, vegetables, and whole grains, and medications as prescribed by a healthcare provider. Avoiding tobacco smoke and limiting alcohol consumption are also important steps in preventing heart valve disease, as these substances can increase the risk of cardiovascular conditions.
Additionally, practicing good oral hygiene and seeking prompt treatment for infections such as strep throat can help prevent conditions like infective endocarditis, which can damage heart valves.
Regular medical checkups and screenings are essential for early detection of heart valve disease and other cardiovascular conditions, allowing for timely intervention and management. Overall, adopting a heart-healthy lifestyle and addressing risk factors can significantly reduce the likelihood of developing heart valve disease and promote overall cardiovascular wellness.
Healthy Lifestyle Choices:
Making healthy lifestyle choices is crucial for maintaining optimal overall health, including heart health. Adopting a healthy lifestyle involves a combination of regular physical activity, balanced nutrition, stress management, adequate sleep, and avoidance of harmful substances. Engaging in regular exercise, such as brisk walking, swimming, or cycling, helps strengthen the heart muscle, improve circulation, and maintain a healthy weight.
A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats provides essential nutrients while minimizing the intake of processed foods, added sugars, and excessive salt. Managing stress through relaxation techniques, mindfulness practices, and hobbies can reduce the risk of heart disease and improve overall well-being.
Adequate sleep is essential for heart health, as it allows the body to repair and regenerate tissues, regulate hormones, and maintain healthy blood pressure levels. Avoiding tobacco smoke, limiting alcohol consumption, and abstaining from recreational drug use are also important aspects of a healthy lifestyle, as these substances can increase the risk of cardiovascular conditions.
By making healthy lifestyle choices, individuals can support their heart health, reduce the risk of developing heart valve disease and other cardiovascular conditions, and enjoy a higher quality of life.
Living with Heart Valve Disease:
Living with heart valve disease can present various challenges, but with proper management and support, individuals can maintain a good quality of life. Adhering to treatment plans prescribed by healthcare providers, including medications, lifestyle modifications, and regular follow-up appointments, is essential for effectively managing symptoms and preventing complications.
This may involve taking medications to alleviate symptoms such as shortness of breath or palpitations, following a heart-healthy diet low in sodium and saturated fats, engaging in regular physical activity within recommended limits, and avoiding tobacco smoke and excessive alcohol consumption.
It’s also important for individuals with heart valve disease to stay informed about their condition, including understanding the type and severity of their valve disease, potential complications, and warning signs of worsening symptoms.
Building a strong support network of family, friends, and healthcare providers can provide emotional support and practical assistance in managing the challenges of living with heart valve disease.
Additionally, participating in cardiac rehabilitation programs or support groups can offer valuable resources, education, and encouragement for individuals navigating life with heart valve disease. While living with heart valve disease may require adjustments and ongoing vigilance, with proper self-care and support, individuals can lead fulfilling lives and enjoy meaningful activities and relationships.
Conclusion:
Heart valve disease presents significant challenges, but with advances in medical technology and a proactive approach to management, individuals can lead fulfilling lives despite the condition.
From early detection through diagnostic tests to a range of treatment options including medications, non-surgical procedures, and surgical interventions like valve repair or replacement, there are many avenues for managing heart valve disease effectively.
Additionally, adopting a heart-healthy lifestyle, including regular exercise, a balanced diet, stress management, and avoidance of harmful substances, plays a crucial role in preventing and managing the condition. By staying informed, adhering to treatment plans, and seeking support from healthcare providers, family, and friends, individuals can navigate the complexities of heart valve disease with resilience and determination.
Ultimately, while living with heart valve disease may require adjustments and ongoing vigilance, it is possible to maintain a good quality of life and pursue meaningful activities and relationships. With continued research and innovation, the outlook for individuals with heart valve disease continues to improve, offering hope for a brighter future.
FAQ’s:
What are the main risk factors for heart valve disease?
Risk factors include advanced age, congenital heart defects, infections, and other medical conditions like hypertension and high cholesterol.
Can heart valve disease be cured?
While some forms can be managed or treated effectively with medications and surgery, not all cases can be completely cured.
How common is heart valve disease?
It is relatively common, especially among older adults, with millions affected worldwide.
What is the life expectancy of someone with heart valve disease?
With proper treatment and management, many people with heart valve disease can live long, healthy lives. However, life expectancy can vary based on the severity of the disease and overall health.
Are there any new treatments for heart valve disease?
Advances in medical technology continue to improve treatment options, including minimally invasive procedures and improved surgical techniques.
“The information provided on this blog regarding medicine prices and side effects is solely based on data collected from public domains. I am not a doctor or medical professional. While I strive to provide accurate and up-to-date information, I cannot guarantee the absolute accuracy or completeness of the data. It is always recommended to consult with a qualified healthcare professional or doctor for personalized medical advice and information. The content on this blog should not be considered a substitute for professional medical guidance. The readers are advised to use the information provided at their own discretion and risk. I do not assume any responsibility for any consequences arising from the use of the information on this blog.
Thank you.”
What are the main risk factors for heart valve disease?
Risk factors include advanced age, congenital heart defects, infections, and other medical conditions like hypertension and high cholesterol.
Can heart valve disease be cured?
While some forms can be managed or treated effectively with medications and surgery, not all cases can be completely cured.
How common is heart valve disease?
It is relatively common, especially among older adults, with millions affected worldwide.
What is the life expectancy of someone with heart valve disease?
With proper treatment and management, many people with heart valve disease can live long, healthy lives. However, life expectancy can vary based on the severity of the disease and overall health.
Are there any new treatments for heart valve disease?
Advances in medical technology continue to improve treatment options, including minimally invasive procedures and improved surgical techniques.